Can Enhanced 3D Bioprinting Techniques Improve Organ Transplant Success Rates?
The future of human healthcare is a tantalizing prospect. Among the numerous scientific breakthroughs, one technique that has shown immense potential is bioprinting. It’s a revolutionary technology that involves printing living tissues as a substitute for actual organs. Like stepping into a science fiction movie, we’re on the verge of being able to print the human heart, kidney, or liver in a lab. But can these enhanced 3D bioprinting techniques improve organ transplant success rates? Let’s delve into this fascinating subject.
The 3D Bioprinting Process
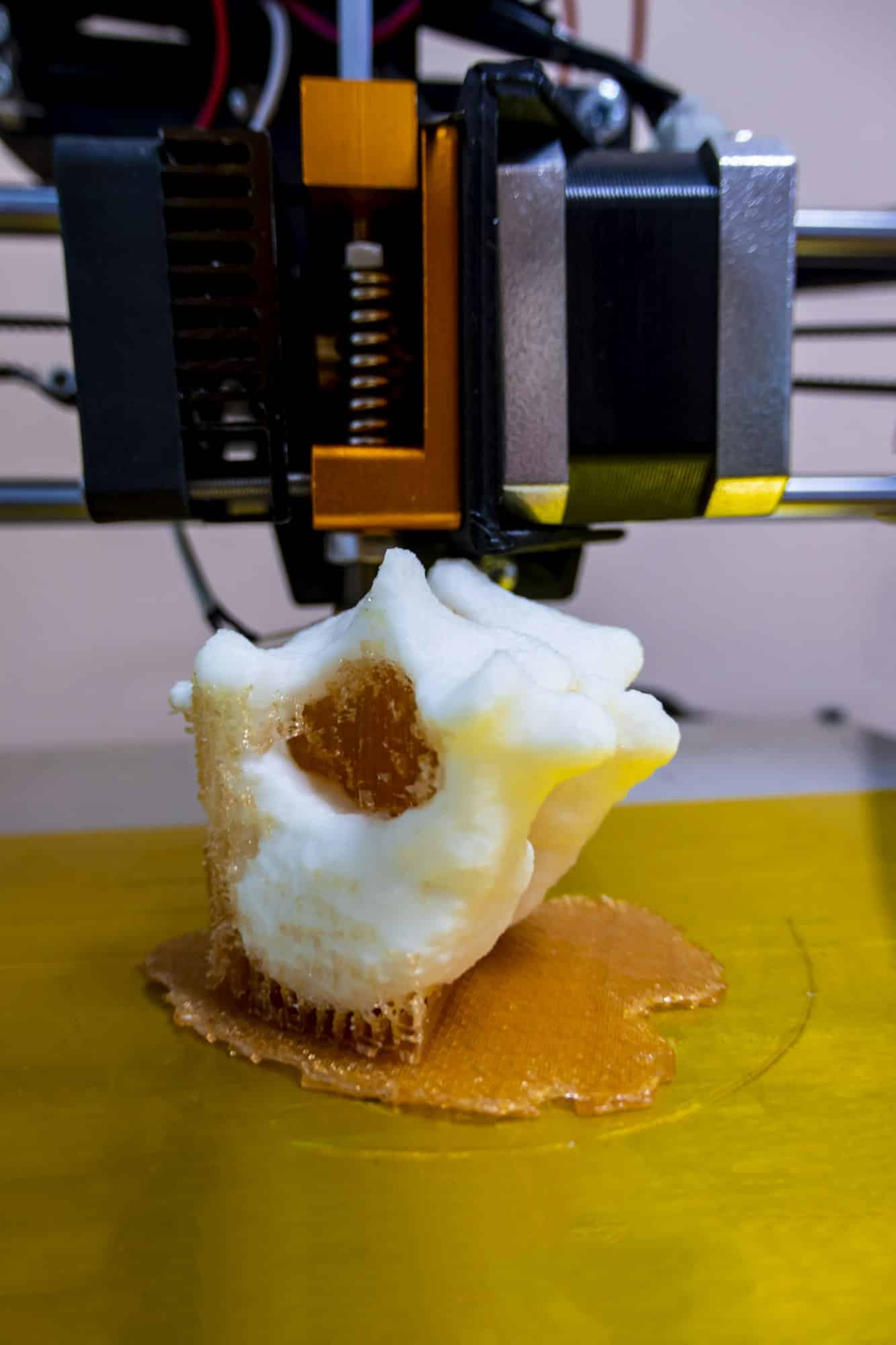
Before we explore the benefits of 3D bioprinting in organ transplants, let’s first understand how the process works. Bioprinting is based on the concept of 3D printing, a method of layer-by-layer fabrication of physical objects from a digital model. However, instead of using plastics or metals, bioprinting uses bioinks, a material typically composed of living cells.
Lire également : What Advances in Haptic Technology Are Making Virtual Reality More Tactile?
The printing process generally involves three steps. First, a digital model of the organ is created, usually based on medical imaging data from the patient (CT or MRI scans). Next, the bioink is prepared from the patient’s own cells or a compatible donor’s cells. Finally, the organ is printed layer-by-layer using a 3D bioprinter.
The Potential of 3D Bioprinting in Organ Transplants
There is a severe shortage of organ donors worldwide. According to the Organ Procurement and Transplantation Network, as of early 2024, over 100,000 people are on the waiting list for a kidney transplant in the US alone. Given the scarcity of donors and the growing need for organs, bioprinting could be a game-changer.
A voir aussi : How Evernex is transforming IT support services ?
The key advantage of 3D bioprinting is that it can create patient-specific organs, using the patient’s own cells. This greatly reduces the risk of organ rejection, one of the major obstacles in organ transplantation. Since the printed organ is an exact match to the patient’s body, it’s far more likely to be accepted without the harsh immune-suppressing drugs that transplant patients usually require.
Furthermore, organs can be printed as needed, which could potentially eliminate the wait times for organ transplants. A scholar could easily find several studies on Google and Crossref supporting the potential of 3D bioprinting in organ transplantation.
The Current State of 3D Bioprinting in Medicine
While the potential of 3D bioprinting in organ transplants is exciting, it’s important to note that we are still in the early stages of this technology. Currently, the most successful application of 3D bioprinting in medicine is in the creation of skin tissue for burn victims and those requiring skin grafts.
Several companies and research institutions are experimenting with printing more complex tissues, like blood vessels and cardiac tissue. However, printing whole organs like the heart, kidney, or liver remains a significant challenge, primarily due to the complexity of these organs. They are composed of different types of cells and have intricate structures and mechanical properties that are hard to replicate.
Yet, progress is being made. Recently, a team of scientists from Tel Aviv University announced that they had printed a small, functioning heart complete with blood vessels, using a patient’s own cells.
The Challenges and Ethical Considerations in 3D Bioprinting
Despite the promising advances, 3D bioprinting is not without its hurdles. One of the biggest technical challenges is vascularization, or the process of forming functional blood vessels within the printed organ. Without an adequate blood supply, the cells in the deeper layers of the organ would die off.
Additionally, 3D bioprinting raises several ethical questions. For instance, if the technology becomes widely available, who will have access to it? Will it only be available to the wealthy? There’s also the question of regulation – who will oversee the process to ensure safety and efficacy?
Also, as with any new medical technology, rigorous testing and trials are required before 3D bioprinted organs can be used in transplants. These trials need to confirm that the printed organs are safe, functional, and can survive for a long term in the human body.
Moving Forward with 3D Bioprinting in Organ Transplants
Despite the challenges, the potential of 3D bioprinting in organ transplants is immense. With continued research and advancements in technology, it’s not unrealistic to envision a future where organ transplants are as simple as sending a digital file to a printer.
Yet, it’s essential that as we move forward, we do so with caution, ensuring that this revolutionary technology is used responsibly and ethically. The day when we can print a human heart or kidney in a lab may still be a few years away, but the progress we’ve made so far is encouraging. The field of 3D bioprinting continues to evolve, bringing us closer to solving the organ shortage crisis and improving the success rates of organ transplants.
Advances in Tissue Engineering Through Bioprinting
Tissue engineering is another key area where 3D bioprinting has made significant strides. The process involves creating tissues in laboratories to replace or support the function of defective or injured body parts. Using bioprinting technology, scientists and researchers have been able to print various types of tissues, including skin, cartilage, and even some forms of vascular tissue.
In a similar vein to organ printing, tissue engineering through bioprinting usually begins with a digital model. The model is then used to guide the bioprinter, which deposits layers of bioink made up of stem cells or other cell types. The printed tissues are then matured in a laboratory before being transplanted into the patient.
One of the most prevalent applications of tissue engineering currently in use is in regenerative medicine. For instance, researchers are using extrusion-based bioprinting to create complex, multi-cellular structures. These printed tissues can then be implanted into patients to promote the regeneration of damaged tissues or organs.
In a remarkable breakthrough, scientists from the University of California, San Diego, managed to print a section of spinal cord that was successfully implanted into rats, promoting nerve growth and improving their mobility.
However, similar to organ printing, tissue engineering through bioprinting faces some challenges. One of the key issues is maintaining cell viability. The process of printing can sometimes damage cells, reducing their ability to function effectively. Therefore, continued research and development are necessary to refine these techniques and ensure the long-term success of tissue-engineered implants.
Conclusion: The Promising Future of 3D Bioprinting in Organ Transplants
The journey of 3D bioprinting in the field of organ transplantation is just beginning. The technology has shown significant promise, with its potential to address the global organ shortage crisis and improve the success rates of organ transplants.
The ability to print organs and tissues in the lab opens up a new world of possibilities for medicine. It offers the prospect of patient-specific organs, reducing the risk of organ rejection and eliminating wait times for organ transplants. The advancements in tissue engineering also hold great promise for regenerative medicine.
However, the road ahead is filled with challenges, both technical and ethical. Issues like vascularization, cell viability, access to the technology, and regulatory oversight need to be addressed. It’s also essential to conduct rigorous testing and trials to ensure the safety and efficacy of the printed organs.
Despite these hurdles, the progress made in 3D bioprinting is encouraging. With continued research, collaboration, and innovation, the day may not be too far off when we can print a fully functioning human organ in the lab. In the meantime, the developments in this field can be followed with interest on platforms like Google Scholar and Crossref.
In conclusion, the potential of 3D bioprinting to dramatically enhance the success rates of organ transplants is immense. It’s a testament to the leaps we’re making in science and technology and represents a bright beacon of hope for countless patients worldwide. As we continue to push the boundaries of what’s possible, the future of healthcare looks increasingly promising.
